The key to treating and preventing heart and vascular disease is understanding how to keep blood vessels functioning normally, rather than deteriorating due to preventable circumstances. Inadequate blood flow is known as ischemia. And ischemia is a major cause of the decline of health known both as disease and as normal aging. Ischemia, the abnormal lack of adequate blood flow has multiple explanations--some of which are identified and many of which are unknown. Discoveries of Dimera that have most significantly formed the path described here are based on rapidly developing insights into balancing gene expression in the blood vessel (cell and molecular medical advances), rather than only symptomatically treating cardiovascular disease. This website focuses on the important topic of blood vessel reactivity, in particular the abnormal increase in coronary artery contraction (vasoconstriction) that occurs in heart disease. Ischemia in the heart severely limits capacity for exercise and as a result, quality of life. Lack of exercise severely accelerates deterioration of blood vessel function and thus leads to ischemia. Dimera offers the new insight that the preventable failure of artery reactivity modulation contributes (along with atherosclerosis) to artery disease of the heart, brain, kidney, bones, and other vital organs.
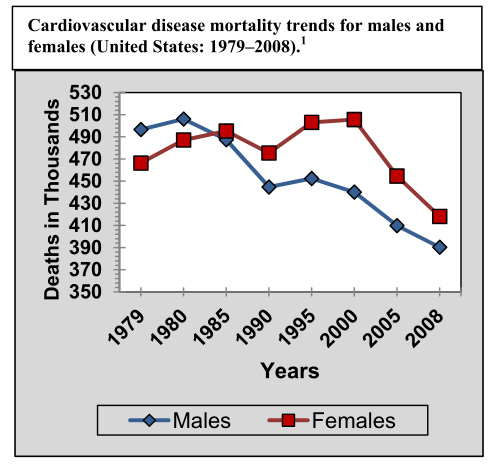
Particularly in women, blood vessel reactivity (rather than just plaques and clots) is vital. Treatment and diagnostics both require recognizing blood vessel reactivity. In cases where blood vessels of the heart (coronaries) do not show the large, surface of the heart plaques or narrowings that are typical in men, diagnosing ischemia is much more difficult. Inadequate blood flow that is caused by small coronary blood vessels (too small to detect by angiography) has only recently been recognized as microvascular ischemic heart disease (IHD). Heart disease signs and symptoms of microvascular IHD include angina pectoris (chest pain of cardiac origin), or otherwise unexplained breathlessness, light headedness, excess fatigue, or symptoms that may seem nonspecific, and at times even minor. However, microvascular IHD is a serious cause for concern as discovered in the long-term, NIH sponsored, Women's Ischemic Syndrome Evalution (WISE) studies cited on the References page. The outcomes of both the combined estrogen and progestin (Prempro) and estrogen only (Premarin) arms of the Women's Health Initiative have brought critically needed attention to the question of how to treat and prevent cardiovascular disease in women. The fact is that the number of deaths of women per year has consistently been greater than that in men for the last 15 years (shown in the first graph below); progress has lagged behind that in men. One reason for this unmet need is the failure to acknowledge different presentation symptoms and causes of coronary disease that are predominant in women. As the graphs below demonstrate, heart disease is not just a man's problem. Every year in the United States, coronary heart disease (CHD), the leading cause of death, accounts for mortality in both women and men, totaling about 500,000 lives. More than 6.5 million women have some form of heart disease, and of those women who survive a heart attack, 46% are predicted to be disabled by heart failure within 6 years.
Chest pain originating from the heart (angina pectoris) in women is typically not triggered by exercise, and is often classified as "atypical" angina, importantly with signs and symptoms different from those usually found in men. Until the last decade, nearly all research data (and thus consequent diagnostic and treatment conclusions) were based on cardiovascular disease characteristics of males. Women often have been denied access to the most advanced medical management if they did not show the typical (exercise-induced) angina pectoris, which is more common and usually correlated with obstructions in men. Confusion persists in the misconception that angina does not increase at the time of menopause--when in fact authoritative epidemiological studies in the medical literature in the last 15 years show there is an increase of >20X in angina incidence during the 10 year time window that encompasses menopause! Different symptoms occur in women, as noted on the Healthy Women page. The standard of medical care for women must improve by acknowledging these data.
A major annual compilation of the evidence upon which future decisions should be based is available in the authoritative publication of the American Heart Association AHA), as "Heart Disease and Stroke Statistics." This PDF file is freely available to everyone at the AHA website, AHA.org. A few data figures from the AHA Annual Report are included below.
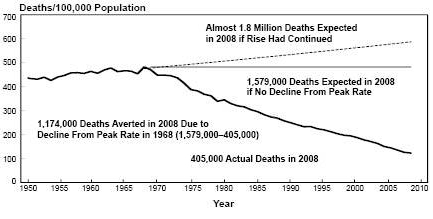
There is now the new and real opportunity to progress beyond the notion that a woman must inevitability spend the last half of her life (from menopause on) with deteriorating cardiovascular function. After 15 years of CV deaths in women greater than CV deaths in men, the trend for women is at last also decreasing (as the graph shows). The improved trend is only the early stage, as Dimera discoveries will allow new treatment and diagnostics. Based on replacement of the deficit of the normal substance that keeps vascular reactivity functioning properly, this new strategy of diagnosis and treatment can decrease total number of fatalities and further improve projected death curves, continuing the advances displayed in the second graph below. Notice that millions of lives in the US alone have been saved as CV medical care improved.
Despite the fact that ischemia is the leading cause of death, there is reason for optimism. Important new blood vessel medical concepts are being pioneered based on cell physiology knowledge. Artery reactivity modulation, although previously unrecognized, is an important, discovery that steroid hormones have a vital homeostatic role for coronary, cerebral, renal, bone, urogenital, and other important blood vessels. Coronary artery hyperreactivity due to falling levels of progesterone, beginning early in perimenopause, has profound quality of life significance, and advancing with age in postmenopausal women. Age-dependent declining levels of progesterone (usually beginning between the 35th-40th birthday) are furthermore hypothesized by Dimera to be important both in women and men. In males, progesterone (secreted by adrenal glands) is also present at levels that modulate gene expression in blood vessels, and the level does fall below threshold in some men.
Coronary hyperreactivity pathophysiology occurs (due to progesterone daily exposure below the threshold) as a functional (not a fixed structural) abnormality, and will not be detected by standard Treadmill Exercise Tests or even by coronary angiography in the catheterization laboratory, and thus may go undiagnosed (which is likely in the small blood vessel malady that is more common in women). Microvascular IHD, particularly that not associated with exercise, has remained practically undetected. Dimera has developed and advocates the concept of using other measures, particularly vasoconstrictor challenges, to permit diagnosis and medical correction of the underlying cause of the abnormality (that we term hyperreactivity) at the genome level (gene expression).
Dimera research presented on the References Cited page of this website (and based on 40 years of NIH funded cardiovascular research focused on the blood vessel wall) has extensively demonstrated (in extensive primate studies) that cardiovascular disease in both women and men may arise due to such functional (non-structural) rather than the pathologically identifiable causes (e.g., atherosclerotic plaques and blood clots). Alternatively stated, reactivity might be as important for causing myocardial ischemia, angina, and heart attacks as fixed plaque or clot types of coronary obstructions. Critically important increases in duration and extent of both coronary and peripheral vasoconstriction which can occur due to even normal stimuli unequivocally add insight to the structural causes of blood vessel disease (Hermsmeyer 2004). Hyperreactivity that is closely correlated with advanced molecular biological understanding of gene expression of the thromboxane-prostanoid (TP) receptor has been demonstrated and verified (please see our several major publications on the References Cited page). Overexpression of the TP receptor appears to be due to a defined severe deficit of a continuous background level of progesterone, and thus the problem can be rectified at the source (the virtues of few or no side-effects) by replacement of the deficit.
Recent recognition of the critical importance of life-long regulation of heart, brain, kidney, bone, and immune functions by steroid hormones represents a major medical advance. Increasingly, Family Physicians, Endocrinologists, Gynecologists, Women's Health Specialists, and other front line practitioners have embraced the concept of non-oral, continuous release steroid hormones which are clearly both more effective and also minimize adverse side-effects. For example, the take-home message for better use of steroid medicines from recent women's health meetings has emerged as start low (in dosage), go slow (in starting or stopping treatment), and use transdermal (not oral) forms of the steroid medicines. Presently, steroid hormone therapies are prescribed predominantly by primary care physicians who represent your most practical access to satisfying ongoing care. Dimera expects recognition by clinicians of progesterone deficits to continue and assume increased importance as continuous replacement by convenient, unit-dose transdermal medicine is found to be highly successful.
The now expected loss of the cardiovascular health due to aging thus may not be inevitable. Instead, blood vessel health that coincides with youthful physical activities (swimming, hiking, tennis, bicycle riding, skiing, golf, basketball, baseball, racquetball, etc) is expected to extend for many decades when attention to the need for progesterone is acknowledged in medical practice. By replacing the progesterone deficit, progesterone-balanced TP expression in the blood vessel wall may greatly extend the number of healthy, active decades of life. From the molecular evidence, it appears that with continued restraint of TP expression at the gene level by continuous transdermal progesterone cream medicine, the duration of peak cardiovascular health will be significantly extended. Dimera predicts such major meaningful, quality-of-life advances in medical care are possible based on this paradigm.
